Pain in the left leg due to disc protrusion. Protrusion of the intervertebral disc. Stages of disease development
Protrusion- a common neurological disease that is a precursor to a hernia. Its main feature is reversibility with proper treatment. More often, pathology develops in the lumbar region due to increased pressure and mobility, depending on the specific load on the spine.
Problems with the spine are the result of injury, osteochondrosis and other problems of the musculoskeletal system. They never appear abruptly, but develop gradually. The spine in the lumbosacral region experiences maximum loads and has increased mobility. Every patient diagnosed with protrusion of lumbar vertebral discs should know treatment methods to prevent the occurrence of a hernia.
Definition of protrusion
Protrusion in the lumbar region is associated with dystrophic and degenerative defects of cartilage tissue. Gradually, a bulging gelatinous body begins to form. It puts pressure on the nerve roots and provokes severe pain. In this case, the fibrous ring is not damaged.
The displacement can be to one side or uniform along the entire perimeter of the vertebra. This displacement disrupts the normal functioning of the spine and causes inflammation and swelling.
Pathology is an intermediate stage before a hernia
A person begins to notice a decrease in muscle tone, problems with coordination and other changes that worsen the quality of physical work.
Video
Protrusion is often confused with a hernia. In the video, the neurosurgeon will explain in detail the features of each pathology.
Causes
Osteochondrosis ranks first among the culprits of protrusion. Almost 90% of the patients examined had degenerative tissue changes associated with improper mineral metabolism and blood supply. The second provocateur is high physical activity. Additional reasons are:
- Heredity, which determines the structure of the spine.
- Low mobility.
- Autoimmune, infectious diseases.
- Physical labor.
- Hormonal imbalances, abnormal metabolism.
- Weak muscle corset, postural deviations.
- Spinal damage.
- Age.
- Excess weight, poor nutrition.
Protrusion of the L 4-L 5 vertebrae is a professional disease of athletes who have had injuries in the past. A person’s age is also important, since after 45 years degenerative changes begin to progress.
Classification
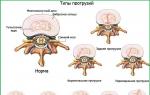
Depending on the shape and direction of the bulge, a classification of pathology has been introduced:
- Circular– squeezing out the corpus pulposum around the perimeter of the vertebra.
- Central located on the posterior surface of the disc and extends to the spinal cord.
- Lateral– left- or right-sided protrusion.
- Diffuse– repeated swelling in different places.
- Dorsal– the corpus gelatinous body seeks an exit into the spinal canal.
The dorsal type is considered the most difficult, as the risk of compression of the spinal structures increases. This may be indicated by numbness and decreased strength of the lower extremities, regular tingling and burning sensations, and paralysis.

Classification is based on the direction of the protrusion
Symptoms
In the first stages of pathology formation, patients note increased fatigue and aching pain in the lower back. If you have such symptoms, it is better to consult and undergo examinations in order to begin treatment in a timely manner.
Subsequently, signs of protrusion will depend on the type and size of the protrusion. It may not appear for a long time or be accompanied by mild pain. But over time, progression occurs, as they say:
- stiffness of movement;
- periodically unbearable back pain;
- low performance;
- muscle weakness.
Most types of protrusion in the lumbar region, except lateral, can be identified by neurological symptoms. A protrusion towards the back from the abdomen is considered dangerous, as the spinal structures begin to suffer.
Separately, doctors identify the cauda equina ligament of nerves. When pressure is applied to this area, more pronounced symptoms and intense pain appear. Patients suffer from problems with urination and defecation.
Diagnostics
The manifestation of symptoms of protrusion should be a reason to visit a physiotherapist or neurologist. The specialist will conduct functional tests and determine the type and exact location of the pathology. The L 4 and L 5 vertebral discs are most often affected.
Instrumental diagnostic methods include X-ray scanning, which makes it possible to analyze the condition of bones and joints. Magnetic resonance imaging and computed tomography will help you choose the right treatment.
Treatment
Treatment of spinal pathology can be conservative or surgical, correcting the disc. Surgery is prescribed as a last resort when conservative methods have not shown good results. Surgery in the lumbar region is undesirable, but if conservative measures are ineffective, it is justified.
At the initial stage, doctors prescribe the following treatment:
- physiotherapy;
- physical therapy with a trainer or independently;
- taking medications;
- manual therapy.

Spinal traction
Drug treatment
Medicines are prescribed during an exacerbation of the disease. This:
- Painkillers a – analgesics, corticosteroids, anti-inflammatory drugs in the form of tablets, ointments and injections.
- Vitamins and chondroprotectors to establish metabolism in tissues. This will speed up the regeneration processes.
- Muscle relaxants and decongestants to eliminate muscle spasms and improve blood circulation. This combination reduces pressure on nerve fibers and eliminates some neurological signs.
Physiotherapy
After the exacerbation is relieved, various courses of physiotherapy are mandatory. Good efficiency is shown by:
- magnetic therapy;
- phono- and electropharesis;
- acupuncture;
- laser exposure;
- massage.
Manual therapy should be provided by a specialist. Qualification and experience will allow the doctor to return the discs to their original position. The effect on the lower back should be gentle, completely excluding sudden movements and direct impact on the affected area.
Spinal traction using a special simulator is effective. It eliminates pain by relieving pressure from the vertebrae. Extraction can be not only dry, but also water. Constant exercise stops the displacement and increase in pressure.
Exercise therapy
The goal of exercises during protrusion is to strengthen muscles, improve motor activity, reduce pain and inflammation. It is better to start training under the guidance of a trainer in a special group, and later move on to independent training. If this is not possible, then you can ask your doctor to create a suitable complex that can be performed at home.

It's best to start with a warm shower to reduce muscle spasms. If any pain occurs, stop exercising immediately. Only systematic exercises give a positive effect. You should not give up exercise therapy halfway through the course.
Standard set of exercises for lumbar protrusion:
- Lie on your back and do scissors.
- Lie on your back: bend your legs, extend your arms. Gently lift your pelvis, resting on your feet and shoulder blades. Hold the top position for a few seconds.
- Working with support (stool). Lie with your stomach on a support and bend forward to stretch your spine. The weight should be between your shoulders and stomach. Lateral traction is done in the same way if you lie on a support with one of your sides.
- Lie on your back with your limbs extended. Try to touch your chest with your chin.
- Walking on all fours with a straight back.
- The most effective will be hanging on the Swedish wall - an analogue of traction.
At first, the exercises are repeated 2-3 times, increasing over time to 6-8 times. The entire training is carried out on a hard surface; the use of a special mat is allowed. After any exercise, rest for 2-3 minutes.
Therapeutic gymnastics should not contain bending or turning that provoke pain. Exercises during an exacerbation period are completely excluded.
Video
The physiotherapist will show you how to properly perform protrusion exercises.
Diet
Cartilage tissue is destroyed due to improper metabolism. A person must control his diet, giving preference to vitamins and minerals. The following will be useful:
- cereals (buckwheat, oatmeal);
- seafood, fish;
- dairy products.
Contraindications include salty, smoked and fatty foods. It is not recommended to use:
- sweets;
- canned food;
- broths and offal;
- confectionery.
ethnoscience
Most folk remedies are aimed at reducing pain. They should not be the only treatment - only complement the main one.
1
Turpentine bath. Fill the bath with water at 40 degrees, add 3 tbsp. mixtures: 10 g baby soap, 200 ml turpentine, 50 g salt, 200 g salicylic alcohol. This mixture stimulates blood circulation and reduces pain. The duration of the procedure is 10 minutes. There are contraindications: cardiovascular pathologies.
Rubbing and compresses made from St. John's wort, birch leaves, Kalanchoe, and wormwood will help alleviate the condition. Before any use of a folk remedy, you should consult your doctor.
Complications
Protrusion can be called a time bomb. It can always cause the following complications:
- compress the nerve endings, causing not only pain, but also paralysis;
- rupture of the fibrous ring with the appearance of a hernia.
You cannot ignore pain in the limbs and lower back, which may be signs of protrusion. Although the pathology develops gradually, it does not stop and will worsen. If treatment is ignored, the person will become disabled.
Prevention
You should not bring the spine to a protusion, and then a hernia. It is important to follow preventive measures that are associated with normalizing lifestyle:
Degenerative pathology of cartilage tissue in the lumbar region is not dangerous. However, pain and stiffness of movement can adversely affect your lifestyle. The next stage after protrusion will be a hernia, which is irreversible and often requires surgical intervention.
(Total 822, today 1)
Thanks to its segmental structure, the spine performs a complex function, providing support and significant mobility.
In many ways, this opportunity is achieved thanks to the intervertebral discs, which together make up about a quarter of the entire spinal column.
With age, degenerative changes occur in bone tissue and intervertebral discs, which lead to their destruction, the appearance of pain and neurological disorders in the spine.
Disc protrusion is the protrusion of the contour of the intervertebral disc beyond the vertebral body without rupture of the fibrous ring.

Fig.: intervertebral disc protrusion
To understand what contributes to the development of protrusions, let us turn to the anatomical structure of our spinal column.
Features of the structure of the spine
Intervertebral discs consist of an annulus fibrosus along the periphery and a nucleus pulposus in the center. The discs are connected to the vertebrae by plates made of hyaline.
The nucleus pulposus is 80% water.

Fig.: structure of the intervertebral disc
The structure is strengthened by longitudinal ligaments that run from the front to the back of the spine. The displacement of the disc in the direction of the spinal canal is prevented by the posterior longitudinal ligament.
When a vertical load occurs, as well as when the body turns, the nucleus pulposus flattens, causing the annulus fibrosus to stretch. At rest, the nucleus takes on its normal shape.
This explains the shock-absorbing function of the spine.

Fig.: spinal ligaments
Another feature of intervertebral discs is that nutrition of the discs through small vessels completely stops by the age of 20-30. As a result of the emptying of the arteries, metabolism occurs only through osmosis and diffusion.
Reasons for development
As most people age, degenerative changes begin to form in their intervertebral discs.
The main reasons for this:
- heredity;
- excessive physical activity at home, at work, in sports (especially among figure skaters, basketball players, volleyball players);
- injuries;
- poor posture.
The severity of predisposing factors largely determines the age of onset of the disease.

Fig.: age-related changes in the spine
The process is usually localized in the cervical and lumbar spine, which can be explained by the significant load on the discs of these areas, resulting from their increased mobility.
Stages and possible consequences
The fibrous ring becomes less elastic and microcracks form in it.
With each subsequent load, the nucleus pulposus protrudes more and more towards the periphery:
- When the outer layers of the fibrous ring are preserved, the disc begins to bulge into the area of its most noticeable thinning - a disc protrusion is formed;
- As a result of a complete rupture of the ring, the nucleus pulposus extends beyond the disc and can even lie freely in the lumen of the spinal canal - a disc herniation is formed.
More often, a lateral displacement occurs in the area in which the spinal root passes.
As a result, compression of the root occurs and pain occurs - discogenic radiculitis.

In rare cases, the protrusion may be located on the back surface in the middle - posterior hernia.
In this case, neurological manifestations depend on the location of the pathological process. In the lumbar region, compression of the roots may occur, and in the cervical region, compression of the cervical spinal cord may occur.
If the integrity of the cartilage plates is violated, the core of the disc can move from the adjacent vertebra - Schmorl's hernia.
The course of this disease is usually asymptomatic.

Fig.: Schmorl's hernia
As a result of degenerative changes in the discs, their sclerosis can occur and the spaces between the vertebrae can decrease – osteochondrosis develops.
Video: formation of intervertebral hernia
Classification and size
Classification depending on the direction of exit of the nucleus pulposus:
- Central. Located in the midline in front of the vertebra.
- Posterior (or dorsal). Located in the midline posterior to the vertebra.
- Left-handed. Located on the left lateral side of the vertebra.
- Right-handed. Located on the right lateral side of the vertebra.
- Foraminal. It is located at the opening from which the nerve root emerges.
- Medial (or median). The disc is split exactly along the radius, the hernia is directed from the center of the vertebra to the periphery.
- Posterior median. It is a type of median or middle hernia, and is directed strictly backward.
- Paramedian. Located next to the median hernia.
- Circular. Circumferential damage to the disc is observed.
- Diffuse. The formation of multiple hernias both at the same level and at different ones.
Classification of hernias by size:
- protrusion – from 1 to 3 mm;
- prolapse or prolapse of the disc – from 3 to 6 mm;
- the hernia itself is from 6 to 15 mm.

Causes and symptoms of the disease
In the cervical region
In addition to age-related changes, whiplash injury - rapid flexion and extension of the neck - as during an accident in the absence of head restraints in the car, is of great importance in the mechanism of development of a hernia in this department.
In case of prolapse on the lateral surface:
- symptoms of root compression develop;
- the onset of the disease is characterized by the appearance of acute pain in the arm, shoulder, and neck;
- pain intensifies during movement;
- Weakness in certain muscle groups and their atrophy are often observed.
When prolapse occurs on the posterior surface, symptoms of spinal cord compression appear:
- pain;
- tingling;
- muscle weakness;
- loss of sensation;
- in severe cases - paralysis.
With a central form:
- there is a decrease in muscle strength in the arms;
- there is uncertainty and awkwardness when walking;
- bladder dysfunction appears;
- in the most severe cases, complete interruption of the spinal cord occurs, which is manifested by a lack of sensitivity and complete paralysis below the level of the spinal hernia.

In the thoracic region
The clinical picture is manifested by severe pain in the heart area, which is a common cause of misdiagnosis of myocardial infarction.
Often the pain intensifies with movement, turning the body, or taking a deep breath. In this case, myositis or neuralgia can be mistakenly assumed.
In the lumbar region
More often, posterolateral hernias are observed, which compress the root at the very beginning.
When central hernias occur, several segments of the spinal cord are compressed, since the loose fragment can move up or down.
More often, the discs between the last lumbar vertebra and the sacrum or between the fourth and fifth lumbar vertebrae are damaged. Only in 5% of cases the disease develops above this level.
Damage in this department is characterized by:
- acute pain in the lumbar region, which radiates to the buttock, back of the thigh and lower leg;
- a sharp increase in pain when bending the body, moving, or straining.
- curvature of the spine, which occurs reflexively due to tension in the back muscles with severe pain;
- the occurrence of pain during sudden movements or lifting heavy objects.

During the examination, pain in the spinous processes is noted, pain intensifies when lifting a straightened leg in a lying position. In some cases, sensitivity in a certain area of the leg may be lost, and the muscles of the limb may be weak.
Symptoms are paroxysmal in nature. Over time, either through treatment or on their own, the symptoms go away or become significantly less severe. Subsequently, attacks of pain are repeated.
Methods for diagnosing the disease
Diagnosing protrusion is not particularly difficult.
Anamnesis and typical neurological symptoms allow us to identify the pathological process and determine its level.

An X-ray examination reveals a narrowing of the distance between the vertebrae at the level of the lesion. If the prolapsed disc begins to calcify, it can be seen on an x-ray.
A complete description of the condition of the spinal column, and the pathologically altered disc in particular, can be obtained using computed tomography or magnetic resonance imaging.
How and with what to treat protrusion of intervertebral discs?
Every disease is easier to prevent than to treat.
Of particular importance in the prevention of neurological diseases of the spine is systematic physical exercise, which is aimed at maintaining correct posture and strengthening the back muscles.

The entire period of the disease can be divided into acute, subacute stages and the stage of remission - the subsidence of the disease.
Treatment in the acute stage
In the acute stage, rest is necessary.
Treatment begins with non-steroidal anti-inflammatory drugs: indomethacin, ibuprofen, piroxicam, etc.
Painkillers and muscle-relaxing medications, countercurrent agents (hypothiazide, furosemide) and B vitamins in large doses are also prescribed.
Thus, drug therapy affects the main links in the development of the disease - it reduces inflammation and swelling, eliminates reflex contraction of the back muscles.
For severe pain, intramuscular injections of dexamethasone, phenylbutazole, lidocaine, cyanocobalamin, as well as epidural and radicular blockades are prescribed.
Traction may be indicated to reduce disc protrusion.

If there is a lesion in the cervical region, it is advisable to use immobilization of the spine using a collar or a special Hallo-west device.
Physiotherapeutic methods
It is carried out in parallel with medication using:
- alternating magnetic field;
- sinusoidally modulated currents;
- ultrasound therapy;
- electrophoresis with novocaine.

Treatment in the subacute stage
After the main pain syndrome subsides, gymnastics, manual therapy, physiotherapy, and massage are used.
The exercises are aimed at:
- muscle relaxation;
- reducing pressure on affected discs;
- eliminating pressure on the spinal cord roots;
- strengthening the back muscles.

The following physical exercises have a positive effect:
- Performing exercises on an inclined board every day for 10-20 minutes is aimed at stretching the spine and increasing the distance between the vertebrae. The pressure on the roots is eliminated and the nutrition of the disc tissue is improved.
- Walk on all fours with your back straight 5 times a day.
- In a supine position, the legs are bent at the knee joints, the arms are straightened along the body. It is necessary to raise the pelvis 3-5 times and hold it in the upper position for several seconds.
- In a position on all fours, simultaneously raise your left arm and right leg, then vice versa. The exercise is repeated 5-6 times.
At this stage, it is necessary to avoid vertical load on the spine and circular movements in the affected area, as they have the most traumatic effect on the disc.
Physiotherapy
- have a relaxing, anti-inflammatory and analgesic effect;
- enhance the effect of medications;
- help in resolving the hernial sac and reducing pressure on the root (with the prescription of enzymes - papain, lekozym, karpazim)
Physiotherapeutic treatment is prescribed in combination with drugs that relax smooth muscles, improve blood flow, and stimulate recovery processes.
The integrated use of physical methods and drug therapy allows you to achieve a positive result more quickly.
To eliminate pain, acupuncture is used.

In remission
In the stage of subsiding of the pathological process, patients are not bothered by back pain.
The main complaint is a decrease in strength in the limb during physical activity, which makes it difficult for the patient to be active in everyday life. In this case, treatment and rehabilitation measures are indicated that are aimed at eliminating spinal defects and preventing relapses.
Constant implementation of therapeutic exercises and sanatorium-resort treatment are used.
Surgical treatment
In the event that conservative therapy does not have a positive result within 3 months, as well as if a prolapsed disc is detected on CT, surgery is indicated.

Symptoms in the presence of which surgery is indicated:
- violation of defecation and urination;
- gait disturbance;
- decreased muscle strength in the arms or legs.
If symptoms of compression of the roots in the lumbar region arise, urgent surgical intervention is performed, since prolonged compression will lead to the appearance of irreversible disorders.
The operation is performed with the patient in the prone position.
When discs prolapse in the cervical region, a posterior approach is used, with removal of the vertebral arches, or anterior (most often), through the bodies and discs.
The anterior approach is preferable, as it makes it possible to remove a disc or formed osteophyte and stabilize the spinal column.
The operation is performed through a transverse skin incision over the affected disc.

The muscles are gradually dissected and provide access to the vertebrae between the carotid artery, esophagus and trachea.
The disc is removed using a cutter: the disc and part of the adjacent vertebrae are removed. Through the formed window, osteophytes are removed and the posterior longitudinal ligament is excised, which helps reduce pressure on the spinal cord and roots.
After the manipulation is performed, the spinal column is stabilized with a small fragment of bone graft taken from the pelvic bone.
After 3 months, the bone fragments grow together.
If necessary, such an operation can be performed at several levels of the lesion. In this case, fixation is performed with a titanium plate with screws.

Fig.: intervertebral disc prosthesis
Removal of protrusion and hernias in the lumbar region can be done using the endoscopic method. This method is characterized by manipulation using special devices through small punctures near the pathological area without providing wide access.
If the operation is performed correctly, the patient can walk already on the first day after the operation.
Folk remedies
- Lubricate the spine with camphor and place a towel soaked in warm milk on it. Keep the compress for 2 hours. After removing the towel, you need to rub camphor oil, massage the healthy and painful area of the back. At night, apply a bandage with a mixture of onion and sugar. Before going to bed, it is advisable to drink warm diaphoretic tea with an aspirin tablet. The next day, repeat all steps. The course of such treatment lasts a week.
- Indian onions, which can be bought from a spice seller, are put through a meat grinder. Add the same amount of fresh honey to the resulting gruel. Rub the mixture into the disc herniation site every day.
- Chatterbox recipe: 100 ml of pharmaceutical alcohol, 1.5 g of novocaine, 1.5 g of anesthesin, 2.5 g of menthol. The resulting mixture must be stored in a dark bottle. Lubricate the affected area 5 times a week.
- Crush 300 g of garlic and add 500 ml of vodka. Leave the tincture for 10 days. apply as a compress at night.
- Mixture: marshmallow root, thyme and wormwood 2 tbsp each, 4 tbsp in a row. Pour the collection with 1.5 water and wait 1 hour, then simmer for 10 minutes on low heat. Use as a compress.
- Collect 3 kg of dandelion stems, squeeze out the juice, first grind through a meat grinder. Add an equal amount of medical alcohol to the juice. Wait 10 days. Heat the resulting mixture and rub it into the sore spot. There may be increased pain, but you must be patient. After a 10-day course, you must take a 10-day break. Repeat treatment 2 more times.
At home
At home, each person must follow certain rules in diet, physical activity, and exercise.
Traditional methods of treatment and manual therapy will come to the aid of every lover of alternative medicine.
Diet
Nutrition for intervertebral hernias requires sufficient intake of nutrients and vitamins into the sick person’s body.
For this purpose, you must eat:
- a large number of apples, pears, raspberries, grapes, nuts, vegetables:
- fish, seafood, nuts, dairy products.

Manual therapy and osteopathy
Osteopathy is a set of manual techniques aimed at diagnosing and treating the disease.
The technique is based on the high sensitivity of the osteopath’s hands to the existing structural changes in the patient’s body.
Manual therapy is contraindicated:
- in the acute period;
- in the presence of infectious and oncological diseases;
- in the presence of fresh injuries;
- with arterial hypertension.
Before starting to use the method, it is necessary to relieve the inflammatory process using medication or acupuncture.
Unfortunately, with a hernia that is 5 years old, the treatment result is likely to be negative. In approximately 22%, it is impossible to completely reduce the hernia.
You should be aware that after any session the hernia may be reduced; the procedure must be stopped.
Repeated treatment of a reduced hernia can lead to relapse of the disease.

Signs of reduction of protrusion:
- cessation of pain;
- no irradiation;
- restoration of sensitivity;
- spreading heat to the hands or feet.
The danger of manual therapy is that if excessive pressure is applied to the sore area, the hernial sac may enlarge.
This phenomenon will be accompanied by a sharp deterioration in general condition.
Yoga
Performing the exercises requires strict adherence to the rules, and its implementation is permitted only under the supervision of an experienced instructor.
Basic principles of yoga:
- If the exercise does not cause discomfort, then it is considered suitable.
- When performing exercises, it is necessary to avoid sudden movements and jumps.
- Twisting exercises should be avoided.
- Gymnastics should be performed 3-5 times a day.
Video: yoga
Prevention of disease occurrence
To prevent the disease it is necessary:
- constantly strengthen your back muscles;
- To unload the back, use special corsets.
FAQ
Are sports activities and this disease compatible?
Professional sports are contraindicated, especially if they involve prolonged vertical load on the spine (basketball, equestrianism, weightlifting).
Instead, it is better to do swimming, yoga and walks in the fresh air.

Is protrusion dangerous during pregnancy?
The danger with disc protrusion is that if exacerbations occur, the use of many painkillers is contraindicated.
Exacerbations during pregnancy occur more often, as the load on the spine increases and a number of hormonal changes occur.
In this case, it is better to seek help from non-drug therapy.
Is it possible to join the army with such a diagnosis?
It all depends on the size, location of the hernial protrusion and the presence of symptoms of dysfunction. In most cases, a herniated disc is a military exemption.
Does the disease occur in children?
Protrusion of intervertebral discs can also be observed in children.
In this case, this is often a congenital pathology and requires the mother and child to contact a specialist doctor.
If protrusion can be cured with conservative methods, then a hernia often requires.
Stages of the disease
Intervertebral disc protrusion has several stages of development, differing in symptoms and treatment methods.
The first is structural changes
characterized by disc protrusion. The nucleus pulposus begins to shift, pressing on the boundaries of the fibrous ring. As a result of this process, a bulge appears, in some cases reaching half the circumference of the disc. In the first stage, a person may experience burning flashes of pain, but this symptom is often absent.
The second is prolapse
At this stage, the nucleus manages to hold the annulus fibrosus, but there is an increase in convexity and pressure on the spine. The patient experiences discomfort, aching pain, and possible burning sensation in the lumbar region.
Third - protrusion
The fibrous ring cannot withstand the load and releases part of the nucleus pulposus beyond its limits. At this stage, severe pain, numbness of the limbs appears, and tissue swelling begins.
Due to the absence of symptoms, treatment of the disease begins only in the second or third stage, when long-term complex treatment is required.

The main reason for this phenomenon is the heavy load on the lumbar spine, which has a significant range of motion.
But usually the occurrence of protrusion is provoked by several reasons, including a sedentary lifestyle, sedentary work, lack of sports activities, metabolic disorders, etc.
The main reasons for the development of lumbar protrusion:
- hereditary structural features of the lumbar column;
- infectious diseases;
- metabolic disorders leading to degenerative processes;
- undeveloped muscle corset and incorrect posture;
- heavy physical activity or a sedentary lifestyle.
Protrusion can also form due to injury, obesity, poor nutrition, or age-related changes in the human body.
Symptoms

The sooner treatment is started, the more effective it will be.
Neglected protrusion can lead to the development of a hernia, surgical treatment and disability.
The disease develops asymptomatically for a long time, sometimes mild pain appears, which many do not pay attention to.
But as soon as the nerve roots are pinched, the person begins to experience:
- stiffness in the lumbar region;
- numbness in toes and feet;
- burning and severe pain in the back;
- dysfunction of the bladder (not observed in all those suffering from protrusion);
- loss of mobility of the affected area and muscle elasticity;
- fatigue;
- discomfort when lifting, bending and sitting.
The first symptoms are mild, but after a few days the pain and discomfort intensify. However, the symptoms in each specific case may be different, depending on the cause and stage of the disease.
Diagnostics
When the first symptoms appear, you should immediately consult a doctor.
He will prescribe an examination: computed tomography of the spine or MRI of the lumbar region. Using the images, the specialist finds the location of the protrusion, its size, makes a diagnosis and prescribes effective treatment.
How to get rid
If you start treatment in the early stages of the disease, it will be quick and painless. Typically, the doctor advises performing a set of physical exercises to restore the health of the lumbar spine, therapeutic massage, Charcot's shower with a contrast temperature of 10 to 45 degrees, the procedure is also called a “shock type” shower.
Conservative treatment methods

In most cases, protrusion is treated with conservative methods; they eliminate pain, tissue inflammation, muscle spasms, strengthen the muscular corset of the spine and help restore its functions.
Drug therapy
It is used during the acute stage of the disease.
The doctor prescribes analgesics that relieve pain and improve a person’s condition, non-steroidal anti-inflammatory drugs, muscle relaxants and B vitamins. The drugs relieve inflammation and reduce compression of the nerve roots.
In some cases, specialists prescribe injections of an anesthetic, cortisone or steroids; they begin to act only after a day and reduce irritation of the nerve roots, but this method of treatment is considered one of the most painful and unpleasant.
Treatment of lumbar protrusion should be comprehensive, therefore, in addition to medications, experts recommend exercise therapy, massage, magnetic therapy, etc.
Exercise therapy is not a new, but effective and popular method of treating protrusion. To get rid of the disease, you need to be patient and willpower. The complex of exercises treated is aimed at increasing motor activity and relieving inflammation. If possible, it is better to attend special courses with a trainer, but self-study is also beneficial.
Massage should only be performed by a professional. In the first days, all manipulations are gentle, without sudden movements. It is important to avoid applying directly to the affected area.
Spinal traction
It can be underwater or dry, both methods allow you to increase the distance between the vertebrae and reduce compression of the nerve roots. With regular traction procedures, subluxation in the intervertebral joints can be eliminated and intradiscal pressure can be reduced.
Laser therapy
Laser therapy heals the human body due to its ability to absorb light. The procedures help regulate metabolism and normalize biochemical processes. Laser therapy can have an analgesic and anti-inflammatory effect, strengthen the body's immunity, and improve tissue nutrition in the affected area.
It is prescribed by a doctor to strengthen the immune system, improve the functioning of the circulatory system and normalize metabolic processes. Magnetic therapy is carried out at any stage of protrusion.
Acupuncture
There is a lot of controversy surrounding this method regarding its effectiveness and the need for prescription. But, as practice shows, acupuncture reduces pain, and the effect of the procedure lasts a long time. But it can only be used as an additional method of treating protrusion of the lumbar spine.
Shock wave therapy
Shock wave therapy is prescribed as an additional or preventive method of treating protrusion. The procedures correct posture, eliminate pressure on nerve roots, strengthen back muscles, and increase their tone.
Surgical intervention

When treating protrusion, surgery is extremely rarely resorted to, as the risks of a hernia, complications and deterioration of the condition after surgery increase.
When is surgery performed?
This is necessary in three cases:
- Conservative treatment did not produce results within 6 months.
- Protrusion develops rapidly; other types of treatment are not able to stop the process of damage to new areas of the spine.
- The fibrous ring has prolapsed too much, which can lead to loss of capacity and risk of disability.
Operations are performed only at the last stage of protrusion, when drug and reflex treatment have not brought results and are no longer effective.
ethnoscience
To ease pain and reduce suffering during protrusion, you can prepare decoctions, tinctures or compresses at home. But it is important to remember that these remedies cannot be the main ones in the treatment of protrusion.
- To relieve acute pain, apply a compress of garlic and honey to the affected area for 20 minutes (the products are taken in a ratio of 1 part garlic to 2 parts honey). This remedy can be replaced by lotions made from Kalanchoe leaves or maclura tinctures.
- Garlic tincture compresses: pour 300 grams of garlic into 150 ml of vodka, let it brew for 10 days. Compresses can be applied for no more than 30 minutes, otherwise the garlic will leave burns on the skin.
- Prepare a bath with turpentine: take water with a temperature of about 40 degrees, add 10 grams of baby soap, a 1% solution of salicylic acid and 1 cup of turpentine. The bath relieves pain and stimulates blood circulation, but it can be taken for no more than 10 minutes.
There are many methods for treating lumbar protrusion, but their choice depends on the patient’s health status, symptoms and stages of the disease.
Exercises

In order for a set of physical exercises to contribute to the treatment of protrusion, it is necessary to carefully consider its formation.
It is important to remember the basic rules:
- In the first days of classes, perform the exercises a minimum number of times, do not strive to do everything to the maximum.
- At first, perform all the exercises in a lying position, preferably on a bed with an orthopedic massage of medium hardness; over time, you can switch to a training mat. Make sure that during exercises there is no pain in the lumbar region.
- Don't rush, do the exercises slowly, resting for at least 2 minutes before each, but you can't drink water at this time.
During exercise, it is necessary to avoid strong turns and bends, which can increase inflammation and disc prolapse.
One of the most effective exercises for lumbar protrusion is considered to be hanging on a wall bars or horizontal bar; at an early stage, you can use a bench for deflections.
These actions reduce pressure on the nerve roots and reduce pain.
To get the desired effect, just do 3 simple exercises:
- Lie on your back, bend your legs slightly, and extend your arms along your body. Tighten your abdominal muscles, but don't hold your breath. Lower your legs, relax, then repeat the exercise. The number of repetitions is 10-12.
- Take the starting position as in the first exercise, slightly raise your upper body, your legs should not change position. Then slowly lower your torso, rest and repeat the exercise at least 10 times.
- Lie on your back, slightly bend your knees, extend your right arm forward and place it on your left knee, bend your left leg and rest your right hand on your knee so that it cannot get closer to your head. Repeat 10 times.
If you do a set of exercises on your own, carefully monitor the correct execution.
If pain occurs in the lumbar region, exercise should be stopped immediately.
Prevention
To prevent severe pain in the spine and long-term treatment, it is necessary to carry out prevention: monitor your posture, regularly engage in physical exercise, for example, swimming, cycling, skiing, etc. If you need to lift weights, you need to know in advance how to do it correctly. Don't forget about weight control and proper nutrition.
If you follow these rules of prevention, your spine will be healthy for many years.
Protrusion of the lumbar spine is an insidious disease that develops asymptomatically for a long time and only in the last stages causes severe pain and significantly limits movement.
As soon as the first symptoms of protrusion appear, you should immediately consult a doctor who will prescribe an examination and effective comprehensive treatment.
Very often, patients complain that their back constantly hurts in the lumbar region, and believe that this is due to.
Of course, the disease provokes pain, but many patients with this diagnosis live without pain. So how can you remove the pain that has arisen and make sure that it does not occur again?

Why does my lower back hurt?
Before finding out how to relieve lower back pain due to protrusion, it is worth considering the mechanism of development of the disease and the causes of pain.
Schematically, the development of the disease proceeds as follows:
- The intervertebral disc becomes thinner and can no longer fully perform its shock-absorbing function. This stage of cartilaginous changes can be painless or accompanied by moderate pain. If at this moment a person seeks medical help, he will be diagnosed.
- Next, the cartilage tissue gradually deforms, and part of it begins to protrude beyond the spinal column - a protrusion occurs. Bulging can occur both outside and inside the spinal column.
It is this protruding part of the vertebral cartilage that causes pain. The mechanism of pain syndrome can be described as follows:
- Due to the influence of unfavorable factors, the cartilaginous bulge causes compression of the nearby nerve process, irritating the nerve endings and causing pain in the affected area of the lumbar region.
- In response to this stimulus, a reflex myospasm occurs, which compresses the vessels and increases the compression of the nerve.
- A vicious circle of pain arises - a spasm, which in severe cases can be broken only by using medications.
Having figured out how protrusion and lower back pain are related, you can select remedies to treat the painful manifestations of the disease.
How to treat
There are several ways to relieve pain from lumbar protrusion. Conventionally, they can be divided into two groups:
- drug therapy;
- non-drug treatment methods.
Drug therapy
To relieve severe pain and relieve muscle spasms, antispasmodics and muscle relaxants are used.
Depending on how much your back hurts due to lumbar protrusion, the method of administering the drug may be:
- Injection (injections, droppers). This method is used only in outpatient settings, all procedures are carried out by medical professionals.
- Tableted. is also possible at home, but their dosage should be selected by a doctor individually, taking into account the characteristics of the disease.
- Local (use of various and). Local administration of drugs is allowed independently, as an “ambulance” for a pinched nerve.
- Nonsteroidal anti-inflammatory ointments, such as Ortofen. The use of this group of drugs not only reduces pain, but also serves to prevent the occurrence of inflammation in the area of myospasm. In addition to non-steroidal drugs, you can use ointments with a warming and irritating effect, such as Apizartron or Finalgon.
- Orthopedic patches, such as Nanoplast, Voltaren, or Nano Patch. Orthopedic patches are convenient because when they are glued to a diseased area of the skin, the medicine is slowly absorbed and a long-lasting analgesic and anti-inflammatory effect is provided.
Non-drug treatment
For lower back pain caused by protrusion, drug treatment is used only in the acute stage to relieve myospasm and reduce the patient's pain.
In the subacute and remission stages, to reduce pain or to prevent its occurrence, the patient is prescribed:

- . Reflex action on certain areas allows you to relax the muscles in the area of pathology and increase blood supply to the tissues.
- . With its help, muscle relaxation occurs in the pain area and, as a result, the intensity of the pain syndrome decreases.
- . An individually selected therapeutic complex helps to increase the elasticity of ligaments and muscles, and increases blood supply to the vertebral cartilage.
- (UHF, laser and other hardware methods) eliminates spasms and swelling, reduces pain.
How to prevent it from getting sick again
Despite the fact that medicinal products have a good analgesic effect, it is better to prevent painful manifestations from occurring.
How to do it? To do this, it is enough to prevent the nerve from being squeezed by the protruding part of the cartilage. As preventive measures it is recommended:
- Do a set of therapeutic exercises regularly. Their implementation helps to increase blood supply to the spine and build up a natural muscle corset.
- During heavy physical activity, wear a lumbar corset, which will prevent displacement of the vertebrae.
These methods will help to cope with back pain due to protrusion, and taking preventive measures will prevent the pain from reoccurring.
Denial of responsibility
The information in the articles is for general information purposes only and should not be used for self-diagnosis of health problems or for therapeutic purposes. This article is not a substitute for medical advice from a doctor (neurologist, therapist). Please consult your doctor first to know the exact cause of your health problem.
I will be very grateful if you click on one of the buttons
and share this material with your friends :)
Among the numerous questions from patients, there are similar groups related to their concerns about their future condition. Can protrusion lead to disability and increase in size if measures are not taken for effective treatment? Can protrusions hurt in principle, or do these pathologies occur without pronounced symptoms? Can a headache occur during protrusion and why does this happen? How is spinal health and high blood pressure related? Can damaged intervertebral discs be cured? All this is just the tip of the iceberg of the questions and doubts that we constantly receive from patients.
The excitement is understandable. After all, what is at stake is an active and fulfilling life, half a day of free and happy movements. Therefore, we will try to clarify all the difficult points and provide a choice to everyone.
Can protrusion go unnoticed?
When pain in the spine appears in the initial stages, this symptom is “written off” as due to excessive physical activity, fatigue, performing unusual work, etc. In fact, only about 5% of people with this condition see a GP for evaluation. This is not surprising, since at the initial stage osteochondrosis does not disrupt the usual rhythm of life and does not interfere with the performance of daily routine duties.
Subsequently, as the intervertebral disc is destroyed, it transforms, flattens, and decreases in height. Accordingly, the pain syndrome intensifies. But the patient has already become accustomed to the presence of constant cutting, pulling, or aching pain in the back. It seems to him that this is a completely normal state.
And when he asks the question of whether protrusion may not produce any symptoms at all and remain unnoticed by subjective sensations, he immediately wants to ask a response question. Do you really not feel stiffness of movement, limited flexibility of the spine and the presence of constant pain?
So, let’s give an intermediate summary as to whether protrusion can be without symptoms:
- no, it cannot, since there is a permanent focus of inflammation in the affected area;
- the prolonged presence of pain dulls the severity of its perception and the data become subjective and not always reliable;
- even if the patient says that there is no pain, it is worth conducting an examination, since many people have a low pain threshold and high expectations for this manifestation of disease;
- a pronounced clinical picture of protrusion can be detected during diagnostic tests, during which the patient will discover a significant decrease in the flexibility and endurance of the spinal column.
If we talk about the data obtained during specialized instrumental examinations, disc protrusion is always clearly visible on the most ordinary x-ray. Another thing is that not every therapist will understand that this is a protrusion and will not prescribe a CT scan.
Can protrusion hurt?
Another common question is whether protrusion can hurt and what signs can be used to determine that it is the one that hurts. We have already discussed above the fact that this condition cannot occur without symptoms. The protrusion itself, of course, cannot hurt. But severe pain occurs due to the fact that as a result of changes in the anatomical structure of the intervertebral disc, compression of the radicular nerves and surrounding soft tissues is observed. It is this factor that causes pain.
Inflammation is a protective compensatory reaction of the body. After all, what happens during protrusion? First of all, this is a decrease in the height of the intervertebral disc. As a result, the vertebral bodies begin to touch. This causes microscopic cracks to appear on their surfaces.
Subsequently, they can provoke the development of growths from salt deposits. At the initial stage, the convergence of the vertebral bodies leads to compression of the soft tissues. There is a threat of compression of the radicular nerves. And this is fraught with disruption of innervation in the parts of the body subordinate to them. The body launches a compensation mechanism. To do this, inflammatory reaction factors are sent to the troubled zone. They provoke severe swelling in the soft tissues, accumulation of lactic acid and blocking of muscles in order to increase the spaces between the vertebrae.
The patient experiences sharp muscle tension in the area of damage to the intervertebral disc, pain and limited mobility. The body fixed the vertebrae due to swelling and muscle tension. Recovery in this state is impossible, since cartilage tissue has the ability to replenish its reserves of fluid and nutrients only through diffuse exchange with actively working muscle fibers.
Roughly speaking, if you want chondroprotectors to work perfectly, then first do an injection, and then go to do therapeutic exercises with the obligatory work of the desired muscle group, or for a massage from an experienced specialist.
Can protrusion cause headaches?
The answer to the question of whether a headache can occur with protrusion depends on the location of this pathology. Most often, migraine occurs with upper localization of intervertebral disc damage. This is either the cervical or cervicothoracic spine. When the protrusion is located in the thoracic and lumbosacral spine, the occurrence of headache is difficult to associate with pathological changes in the spinal column.
Why is that? Let's try to explain:
- large cerebral blood vessels pass through the cervical spine - when they are damaged due to the transformation of the discs, there is a deficiency in the supply of oxygen and glucose to the structures of the brain;
- This is also where the radicular nerves originate, which regulate the functioning of the autonomic nervous system, which is also responsible for the tone of blood vessels and blood pressure level - with pathological changes, this function is disrupted and hypertensive crises can occur and vegetative-vascular dystonia develops;
- muscle tension headache occurs with prolonged spastic tension of certain groups of neck muscles, blocking the normal blood supply to the structures of the brain;
- pressure on the spinal cord can cause sympathetic vasospasm.
This is not a complete list of reasons why a headache may occur with protrusion in the cervical spine. It is worth knowing that 65% of ischemic strokes of the posterior lobes of the brain are caused by cervical osteochondrosis and its complications, such as protrusions. Therefore, you should not delay treatment.
Can protrusion disappear completely?
It often happens that patients who just a few weeks ago came to us with severe symptoms and characteristic radiographic images come back again. And they ask the question whether the protrusion will disappear forever or is it a defect in the film used for their re-examination. The answer is yes, protrusion can be easily treated using manual therapy techniques. Yes, she may disappear. As for whether it’s permanent or not, we find it difficult to answer, since much will depend on the patient himself.
In our manual therapy clinic, doctors do everything necessary to fully restore the health of the spinal column. For this purpose, the most advanced techniques are used and an individual course is developed. During traction traction, osteopathy sessions, massage and reflexology, we create conditions for the complete restoration of the intervertebral disc. Then, by carrying out kinesitherapy and therapeutic exercises, we strengthen the muscular frame of the back and create conditions to prevent destruction of the cartilage tissue of the fibrous ring in the future.
Well, in order to maintain his health, the patient must follow the recommendations that are individually given to him by the chiropractor, who monitors the process of his treatment.
And disc protrusion - it’s not that it can, it should disappear with a properly developed and carried out course of treatment. This is exactly what our work is aimed at.