Posterior central herniation of the intervertebral disc L3 4. Causes, symptoms and treatment of disc herniation L4 L5. How does a bulge form?
Disc herniation l4 l5 is a disease that represents the protrusion of part of the intervertebral disc into the spinal column. 50% or more of all hernias occur in the lumbar spine, which is explained by the heavy load on this section. The medical nomenclature is as follows: the letter “l” means lumbar, lumbar. 4 and 5 are the serial numbers of the vertebrae.
A herniated disc l4 l5 means that the bulge is located between the fourth and fifth lumbar vertebrae.
The L5 hernia itself is not as dangerous as its consequences. The main threat is compression of part of the spinal cord and exiting nerve roots, which causes a certain clinical picture. It is believed that this hernia is the most dangerous among all spinal protrusions.
In a narrow sense, an intervertebral hernia is a pathology of the musculoskeletal system associated with partial migration of the central core of the intervertebral disc with subsequent rupture of the peripheral tissue of the ring.
Brief Anatomy of the Vertebrae and Disc
The lumbar spinal column contains 5 vertebrae connected to each other by an intervertebral disc. The 4th and 5th vertebrae are the last in the section, followed by the sacral section. The structures located between the vertebrae are called discs. They perform the function of absorbing pressure, preventing the vertebrae from touching each other closely, protecting them from destruction.

The disk itself consists of an outer peripheral part and an inner central part. The periphery consists of the fibrous ring, and the inner part consists of the nucleus pulposus, which is filled with a gel-like liquid.
The spinal column itself consists of 34 vertebrae, in which in their center there is a long canal where the spinal cord lies. The peripheral part of the nervous system is extremely sensitive to all types of damage.
The actual hernia is formed when the peripheral part of the disc is destroyed, and the gel-like part of it passes through the crack. During the process of forming a bulge, the disc simply becomes wedged into the spinal cord, causing symptoms of the lesion.
At the physiological level, physical irritation of the nervous tissue occurs; nerve impulses are artificially created and sent in excessive quantities to a certain area of the body.
Stages of formation
During its development, protrusion goes through four stages:
- Protrusion stage. A small crack forms in the area of the annulus fibrosus, through which part of the nucleus can pass. If at this time the influence of provoking factors is stopped, the “wound” will heal. At this time, the bulging diameter is up to 3 mm.
- The second stage is disc protrusion. The nucleus pulposus begins to partially shift into the area of the intervertebral canal. At this stage, the hernia is already beginning to compress the nerve roots and slightly the spinal cord. The muscles go into a state of spasm. Dimensions reach 5 mm.
- Extrusion – increased protrusion of the disc. The outer shell of the disc ruptures. During this stage, the patient experiences severe pain in the lumbar region.
- Loss of the central part of the disc - the nucleus. A full-fledged hernia is formed. Severe compression of the spinal cord and nerve fibers occurs. There is a possibility of developing inflammatory processes that can spread to the entire part of the peripheral nervous system. Gradually, the disc undergoes calcification - it hardens, completely losing its function.
Reasons for development
There are a number of factors influencing the formation of a hernia:
- a sedentary lifestyle, when a person’s back muscles weaken, atrophy and do not support the skeleton;
- inadequate loads on the back. This mainly applies to people whose lives are connected with hard work and professional sports;
- spinal diseases: scoliosis, kyphosis or lordosis. They are manifested by irregular bends to the side, back and forward, respectively;
- injury to the spine or individual vertebra: fracture, bruise, dislocation;
- excess body weight, when the load on the intervertebral disc increases significantly;
- people whose age ranges from 30 to 50 years. With age, the body's compensatory capabilities weaken, ligaments and muscles become depleted;
- genetic predisposition to weakness not only of the ligamentous system, but also of the musculoskeletal system and muscles.
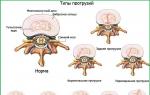
Varieties
Hernia of the lumbar spine is famous for its great variability.

So, the following types are distinguished:
- Median disc herniation l4 l5 . It is characterized by the median location of the protrusion relative to the central axis of the spinal cord.
- Diffuse disc herniation l4 l5 . Its distinctive features: uneven distribution of the central part of the disc along the lumen of the spinal canal.
- Foraminal disc herniation. This subtype is characterized by a specific location. The hernia grows at the site where the nerve roots exit the spinal cord. In clinical practice, symptoms of damage not so much to the spinal cord as to the branching roots predominate. Type: paraforaminal hernia - bilateral protrusion.
- Paramedian disc herniation. It is characterized by a uniform distribution of hernial tissue relative to the center of the peripheral nervous system. Paramedian pathology can be left- or right-sided. One of the subtypes is median paramedian hernia.
- Circular disc herniation is a herniated intervertebral disc, parts of which surround the spinal cord at the lumbar level.
- Dorsal hernia . It is characterized by the direction of the protrusion towards the canal of the spinal column. The dorsal hernia is in close contact with the spinal cord.Dorsal disc herniation has a number of subtypes, including:
- dorsal diffuse disc herniation – uneven distribution of gel-like fluid behind the spinal cord; posterior diffuse disc herniation most often occurs against the background of degenerative bone diseases;
- dorsal median hernia located exactly behind the spinal cord along the central axis; posterior median hernia has a favorable course.
Clinical picture
Symptoms of hernia pathology appear already in the first stages of development. So, a person begins to feel pain in the lower back. The pain syndrome intensifies when the patient engages in physical labor and exercise.
There is a direct proportion: the larger the hernia, the more pronounced the pain.

In addition, the following signs are present:
- swelling in the lower back, shooting and aching pain;
- pain syndrome tends to spread to the pelvis and lower limbs, buttocks;
- all types of sensitivity are impaired: temperature, tactile; the patient complains that he perceives sensations worse;
- paresthesia in the form of numbness, tingling, and a sensation of goose bumps appearing on the skin;
- autonomic disorders: sudden cold or warming of the skin, excessive sweating;
- functional disorders of the pelvic organs: impaired urination, difficulty defecating; in men, libido decreases, erectile function is weakened, in women – birth defects;
- weakness when extending the foot.
Diagnostics
Instrumental diagnostic methods are of great importance in making a diagnosis.
Such as:
- Magnetic resonance imaging.
- CT scan.
- X-ray diagnostics.
- Myelography.

Based on the data after the procedures, a final diagnosis is made and treatment begins.
Treatment
Treatment of the disease is based on conservative treatment and surgery. The first type of treatment includes drug therapy and physical therapy.
Medicines include:
- painkillers;
- anti-inflammatory drugs;
- muscle relaxants;
- vitamin complexes;
- chondroprotectors.
All these substances are aimed at relieving pain, relaxing muscles, eliminating and preventing inflammatory processes. Also, drug therapy is intended to regenerate connective tissue and increase the nutrition of bone and cartilage tissue.
After doctors have relieved the pain, the stage of adding secondary treatment methods begins.
This includes:
- physiotherapy: treatment with long-wave radiation, use of ultraviolet rays;
- activity in the pool;
- massage sessions, medical staff teaches the patient self-massage;
- physical therapy and gymnastics.
Gymnastics is designed to restore the patient’s muscle balance, which is achieved through a series of exercises prescribed by the attending physician. It is not recommended to do the exercises on your own. Therapeutic exercise involves stress on the abdominal muscles, push-ups.

Surgical treatment consists of eradicating the cause of the pathology.
Today, the following types of surgical intervention are relevant:
- Microdiscectomy – removal of the protruding part of the disc. This is considered to be the most effective healing method.
- Endoscopic intervention options . They are carried out through small punctures through which small tubes are inserted, with the help of which the surgeon removes the hernia.
Surgery has a number of advantages over conservative therapy:
- the operation is painless, the therapeutic effect occurs almost immediately, and the patient gets back on his feet within a few days;
- the patient quickly gets rid of suffering;
- the probability of relapse drops to 5%.
The disadvantages of the operation include the insignificant risk of infectious complications during the surgical intervention itself.
For a hernia at the L4-L5 level, in addition to the symptoms of sciatica described above, symptoms such as problems with straightening the big toe due to muscle weakness and potentially the symptom of “foot drop” are characteristic. Numbness and pain may be felt in the top of the foot. Pain from the lower back often radiates to the buttock.
Causes
An intervertebral hernia in the lower back may appear due to injury or incorrect posture when lifting a heavy object (leaning down on straight legs), or it may occur spontaneously. Aging plays a major role in the formation of a hernia. With age, intervertebral discs lose water and nutrients and become less elastic and more fragile. The outer lining of the disc may thus become “weakened” and no longer be able to hold the nucleus pulposus in the center. Genetic predisposition, smoking, work habits and a number of other factors can lead to early degeneration of intervertebral discs.
Intervertebral hernia most often occurs in people from 30 to 50 years old, although middle-aged and elderly people also often suffer from intervertebral hernia, especially if they are actively involved in sports or have a job that involves systematic lifting of heavy weights or static postures (working at a computer, sewing machine, work of a welder, surgeon, etc.) Intervertebral hernia of the lumbar spine is one of the most common causes of low back pain, combined with pain in the leg, and is 15 times more common than hernia of the cervical spine, although with the advent In our life of computers, this ratio is changing, as the number of hernias of the cervical spine and, accordingly, early strokes is growing.
Diagnostics
Diagnosis of intervertebral hernia begins with a visit to a neurologist. The doctor will take a complete medical history of the patient, information about injuries and illnesses, and determine whether any features of the patient's lifestyle may cause pain. After collecting information about the patient, the doctor conducts a physical examination. The examination is carried out in order to determine the source of pain and determine the severity of symptoms such as muscle weakness and numbness, if any.
After examining and making a preliminary diagnosis, the doctor usually refers the patient to a radiographic examination. Such a study can be radiography, MRI (), CT (computed tomography), myelography or electromyography. Based on the data obtained, the issue of treatment methods for the patient’s problem will be decided.
MRI is a non-invasive test that uses a magnetic field and radio waves to create three-dimensional detailed pictures of both the bone and soft tissue of the spine. Unlike X-rays, MRI images clearly show nerves and intervertebral discs. MRI can determine the location and size of the herniated disc, as well as the presence or absence of nerve root compression. MRI can also show bone growths, spinal cord tumors, or abscesses.
Myelography is an x-ray using a contrast agent that is injected into the spinal canal during a spinal puncture. In the images obtained using this study, you can see intervertebral hernia, bone growths, spinal cord tumors, and abscesses. The quality of images obtained in this way is much inferior to the quality of MRI images. Injecting a contrast agent may not be safe for the patient. Myelography as the main diagnostic method is used in countries that cannot afford to buy a sufficient number of MRI machines.
A CT scan is a safe, non-invasive test that uses X-rays and a computer to produce two-dimensional images of the spine. CT is somewhat similar to MRI, but the quality of CT images is inferior to that of MRI. CT is often used as a replacement for MRI in cases where MRI is not possible for some reason. The intervertebral disc is not visible on CT and it is impossible to determine the exact size of the disc herniation using CT.
Electromyography and nerve conduction studies. EMG measures muscle response to electrical stimulation. To do this, small needles are placed into the muscles, and the measurement results are recorded on a special device. A nerve conduction study is similar to an EMG, but it measures how well nerves transmit electrical signals from one end of the nerve to the other. These tests can detect nerve damage and muscle weakness. Tests are used for differential diagnosis of spinal cord diseases.
Radiography uses X-rays to take pictures of a patient's bone tissue, which can help doctors determine changes in the alignment of vertebrae, arthritis, bone spurs, or fractures. It is impossible to diagnose a herniated disc using this test alone.
Treatment
Conservative (non-surgical) treatment of intervertebral hernia may include taking painkillers and anti-inflammatory drugs, non-stress traction of the spine, various sets of therapeutic exercises, various types of therapeutic massages, etc. With a systematic approach to treatment, 80% of people with lower back pain already return to health after about 6 weeks. usual way of life. If for some reason the patient does not respond to conservative treatment, the doctor may recommend surgery.
1) Conservative methods
Taking medications: Depending on the severity of the situation and the severity of symptoms, the doctor may prescribe various painkillers and anti-inflammatory drugs, muscle relaxants (if muscle spasms are present) and steroids. However, steroids can cause serious complications (diabetes mellitus), prescription of NSAIDs and stomach and intestinal ulcers. At the same time, drug treatment for medium and large intervertebral hernias, as well as for a narrow spinal canal, usually does not bring results.
Non-stress spinal traction: this method of treatment allows you to partially restore nutrition and, accordingly, the condition of the intervertebral discs, as well as remove or ease pressure on the nerve by increasing the distance between the vertebrae. Spinal traction is practically the only method of treating disc herniation that acts on the cause of the disease. Since the beginning of the development of intervertebral hernia is a decrease in the intervertebral distance (osteochondrosis of the spine).
Therapeutic gymnastics: strengthens the deep back muscles, promotes the development of correct posture and muscle corset.
Medical massage: helps relax the back muscles and relieve muscle spasms.
2) Surgical treatment
Surgical treatment for intervertebral hernia of the lumbar spine can be recommended in three cases:
- if the patient responds poorly to complex conservative treatment;
- if the patient experiences an increase in symptoms after complex conservative treatment;
- if the patient has signs of nerve damage, such as muscle weakness or loss of sensation in the leg. In other cases, doctors should not recommend surgical removal of an intervertebral hernia.
Today there is practically not a single person who does not complain of periodic lower back pain. They can be a consequence of banal physical fatigue, prolonged exposure to a static sitting position. But such a symptom often indicates the development of serious problems with the spine. Protrusion of the l5 s1 disc is a lesion of the lumbar region. If left untreated, it can lead to the development of a hernia, requiring surgical intervention. But here the consequences can be completely different.
L5 s1 protrusion is when the specified disc extends beyond the spine. In this case, the fibrous ring remains intact. If it ruptures, an intervertebral hernia appears. The protrusion can vary in size - from 1 to 5 mm. If it is not pinched, then symptoms do not appear. A person may not even be aware of the problem of l5 s1 protrusion for a long time.
Most often, this pathology is a complication of osteochondrosis, in which destruction of cartilage tissue occurs, and then the vertebrae themselves. The lumbar region suffers most often, as it experiences the maximum load.
Causes
Disc protrusion l5 s1 does not occur on its own. Often the pathology is a consequence of an incorrect lifestyle or delayed treatment of osteochondrosis. There are other reasons for the development of pathology:
- Deformation of the spinal column (congenital or acquired).
- Back injury.
- Changes in the l4-l5 vertebrae due to age-related degenerative processes.
- Congenital skeletal pathologies.
- Osteoporosis.

- Weak activity, constant sitting position.
- Too much body weight.
- Chronic diseases of bones or muscle structures.
- Poor blood circulation in the lumbar region, as a result of which the vertebral discs do not receive proper nutrition.
The pathological process can be triggered by severe local or general hypothermia of the body, constant exposure to stressful situations, poor nutrition, and excessive drinking and smoking.
How does a bulge form?
Protrusion of the l4-l5 discs develops gradually. Along this path, the disease goes through several stages:
- Microscopic cracks appear on the fibrous ring, however, it continues to remain intact. No protrusion has yet been observed. At this stage, symptoms may not appear, although sometimes flashes of pain are felt, which disappear on their own within a short time.
Neurologist Ignatiev Radion Gennadievich will tell you more about protrusions:
- A small protrusion appears (1-2 mm). At the same time, the fibrous ring continues to deteriorate. The pain syndrome becomes long-lasting and medications are required to relieve it. The patient's physical activity is limited. Discomfort is felt not only in the l5-s1 disc area, but also spreads to other areas of the body.
- The third stage of protrusion is characterized by rupture of the fibrous ring. The disc bulges even more. The pain syndrome becomes very intense, and it is not always possible to relieve it with standard analgesics. If nothing is done at this stage, the patient will develop a hernia. If it becomes pinched, partial or complete paralysis of the lower extremities may occur.
There is no need to put off treating the disease for too long. It is better to play it safe and get tested as early as possible, especially if there is a genetic predisposition to diseases of the musculoskeletal system.
Forms of pathology
Protrusion of the L5 intervertebral disc varies. It all depends on which direction it moves.
Table 1. Forms of pathology
| Type of disease | Characteristic |
| Circular disc protrusion | This protrusion of the l4-l5 discs is more common than others. The protrusion occurs in a horizontal projection in a circle. Its size often reaches 4mm |
| Dorsal disc protrusion | The presented pathology is also common. In this case, the protrusion occurs towards the spinal cord. In this case, the fibrous ring does not rupture completely |
| Central protrusion of discs l4-l5 | The disk here goes towards the “horse tail”. It is here that there is a significant plexus of spinal nerves |
| Here, too, the disc protrudes towards the spinal canal. At the same time, it is destroyed by 25-50% of its volume | |
| Paramedian protrusion | Such a lesion in the l5-s1 segment affects the nerve roots of the sacral spine. At the same time, the right-sided version of the protrusion is much more common than the left-sided one. |
| Foraminal protrusion | It is characterized by damage to the lumbar nerve root. When it is pinched, a person feels severe pain |
Depending on what form of pathology is observed in the patient, appropriate treatment is prescribed. Posteromedian protrusion is considered quite complex, as it poses a threat to the spinal cord.
Symptoms of protrusion
Regardless of what form of pathology develops in a person, it must be treated. In the later stages of development of disc protrusion l4-l5, l5-s1, the following symptoms appear:
- , which becomes more intense when moving or making sharp turns.
- Spread of discomfort to the legs, hip, intercostal spaces.
- Muscle tissue spasms.
- Numbness of toes and hands.
- Changes in blood pressure.

As the pathology develops, a person may experience dizziness
- Muscle weakness.
- Head pain, dizziness.
- If the pathology is too advanced, then a person may have difficulty urinating.
- Painful sensations that appear after raising a straight leg.
- After the onset of pain, the patient may hear a crunch in the spine.
The symptoms of l4-l5 disc protrusion cannot be called specific, since they can also be caused by other pathologies. That is why the diagnosis of the disease must be differential. It is better to start treatment as quickly as possible in order to prevent the development of complications of disc protrusion l4-l5 and l5-s1.
Diagnostic features
What L4-L5 disc protrusion is is already clear, but it should be correctly distinguished from other pathological processes occurring in the spine. This will require a thorough diagnosis.
The examination involves performing the following procedures:
- External examination of the patient, as well as recording of his complaints. Palpation will allow you to feel the protrusion.
- Radiography. It will detect changes in the vertebrae: the proliferation of osteophytes, damage to the surface of the vertebrae.

Ultrasound of the vessels of the affected area of the spine
- MRI or CT. This study will provide maximum information about the condition of the vertebrae, discs, soft tissues, nerves and blood vessels.
- Ultrasound. Ultrasound will make it possible to assess the condition of blood vessels and soft tissues.
The pathology must be diagnosed as early as possible. Otherwise, large areas of the spine will be involved in the pathological process, and the innervation of internal organs will be disrupted. The result of inaction or improper therapy will be a person’s disability, loss of ability to work, and deterioration in quality of life.
Treatment
If you do not pay attention to the protrusion in a timely manner, then in its place in the area of the l5-s1 vertebra a hernia will form, which already poses a danger to human health. The type of therapy and its intensity largely depend on the size of the protrusion.
Traditional and physiotherapy
Medications for l4 protrusion are used only to eliminate pain and possible inflammation. Otherwise, preference is given to massage, physical therapy, and physiotherapeutic procedures.
As for medications, treatment will require analgesics (Ketanov), NSAIDs (Diclofenac), vitamin complexes (based on B vitamins), muscle relaxants (Sirdalud, Mydocalm). Medicines can only eliminate symptoms. But without physical activity and following the doctor’s instructions, they will not get rid of the very cause of the symptoms.

Diclofenac is a drug with analgesic and anti-inflammatory effects. The average price in pharmacies is 50 rubles.
Massage helps restore lost muscle tone and relieve pain. Manual therapy techniques allow you to use not only bone structures, but also soft tissues. An experienced specialist will be able to correct the location of the vertebrae relative to each other. The therapist will realign the displaced parts of the spine. This procedure is not safe, so you should make sure that the person operating on the patient’s body is qualified. This type of treatment is not used in an acute condition, or if the diagnosis is not clearly established.
Table 2. Physiotherapeutic procedures
| Type of procedure | Characteristic |
| Mud therapy | Baths and applications are done already at the stage of recovery of the body after the acute process has been eliminated. They help restore blood circulation and improve tissue regeneration |
| Electrophoresis | Electrical impulses promote deeper penetration of medications, so therapy is more effective. The procedure causes virtually no side effects and can last for a long time |
| Magnetic therapy | The magnetic field allows you to quickly eliminate pain and promote tissue regeneration |
| UHF | The procedure improves metabolic processes, destroys salt accumulations in joints, and eliminates pain. |
| Laser therapy | It improves biochemical processes in the body, which allows tissues to recover faster |
Folk remedies to get rid of protrusion of the l4-l5 and l5-s1 discs do not bring serious benefits, although in some cases they help to somewhat reduce the intensity of pain.
Physiotherapy
Gymnastics is the main method in complex therapy, which allows you to strengthen the spinal muscles and reduce protrusion. The mobility of the lumbar region is also restored. However, some exercises cannot be used if the l4-l5 and l5-s1 discs are affected. Performing movements should not be accompanied by pain. It’s better not to put unnecessary strain on your lower back.
If a person has already started doing gymnastics, then it needs to be continued. There should be a break of 1-1.5 minutes between each exercise, especially in the first days. During physical exercise, the corset or bandage must be removed.
A set of exercises that can significantly improve the patient’s health:
The following complex will be useful:
- In the position on your stomach, you need to alternately bend your knees and lift them. Next, the foot is covered by the hand and pulled forward.
- Now you can roll over onto your back. One leg should be bent at the knee and pulled towards the torso. After this, an exercise is done that is similar to pumping up the abs, only the tension is applied not to the abdominal muscles, but to the back muscles.
- The last exercise is performed in a side position. The limb must be bent and pulled towards the body. The movement is repeated 4-5 times.
Gymnastics is done on a soft mat. If the patient feels even slight discomfort, then the exercises should be stopped. You can perform the exercises at home, but the complex is selected by a specialist individually for each patient.
When is surgery necessary?
Median (discs l4-l5 and l5-s1), as well as other types of pathology presented, are not always amenable to conservative and physiotherapeutic treatment. In particularly difficult cases, in the presence of a hernia or severe deformation of the spinal column, surgery may be prescribed. It is indicated if the protrusion has developed to such an extent that changes in the spine are irreversible.

Laser vaporization burns out a herniated disc with minimal intervention
In general, the affected disc can be removed using a scalpel. But there are gentle types of operations that do not require a long recovery period. Among such operations are:
- Hydroplasty (the affected vertebra is exposed to a high-pressure water jet, which washes away all parts of the destroyed disc).
- Laser burning of the damaged part. But the procedure will be effective only in the early stages of pathology development.
- Vaporization of the affected disc with cooled plasma.
No matter how safe the operation may seem, it is better not to go through with it.
Disease prevention
Dorsal disc protrusions l5-s1 can develop in any person. Even a child can be affected if he or she is seriously involved in sports and exercises excessively. However, if you monitor your health, this pathology can be prevented. To do this, it is better to follow these preventive measures:
- Eat properly.
- Move more: ride a bike, swim, walk, do morning exercises. If a person has a sedentary job, then he should warm up every hour.

- Watch your posture.
- Periodically undergo preventive examinations, as well as attend massage courses.
Protrusion can be cured without resorting to medications or surgery. But for this it must be detected at an early stage of development.
Article publication date: 06/03/2015
Article updated date: 11/08/2018
More than 50% of all cases of intervertebral hernia formation occur in the lumbar spine, and most often in its last segment, formed by the L4, L5 vertebrae and the disc between them. L4 L5 disc herniation accounts for 46% of the total number of occurrences of this pathology in the lumbosacral spine.
The color in the diagram highlights the area of pain distribution when various intervertebral discs of the lumbar spine are affected
When a protrusion forms in this segment, there is a danger of compression (pinching) of the l5 nerve exiting at this level, and, as a consequence, disruption of the innervation of the limb on the affected side, a decrease in sensitivity and range of motion, and the development of muscle atrophy.
Disc herniation of the L4 L5 segment is the most dangerous of all types of intervertebral hernias. It can provoke disruption of the pelvic organs, limitation of motor function, and lead to partial or complete paralysis.
Symptoms of the pathology appear almost from the very beginning of the formation of a hernia: a person is tormented by aching and shooting pains in the lower back and leg, he constantly feels numbness in the lower leg and foot, the leg bends poorly at the knee, and the foot does not fully perform its functions when walking.
Some good news: the development of modern medicine makes it possible to get rid of the unpleasant symptoms of a L4 L5 disc herniation without resorting to surgery. And further compliance with the regime of physical activity and nutrition allows you to restore damaged tissue by 80%.
Causes of L4 L5 disc herniation
The lumbar vertebrae are much larger than other segments of the spine and wider in diameter than in height. This feature is explained by the heavy load that the lumbar region experiences continuously throughout the day. Having no supporting structures other than the muscular frame, the vertebrae of group L (Lumbar - lower back) take on the weight of the entire body, since the center of gravity falls on them. And at the same time they allow the body to turn in different directions with a large amplitude.
Most of the severity is experienced by the last vertebral segment, consisting of the L4 L5 vertebrae and the disc between them. With a slight disturbance in the nutrition of the disc or a change in the structure of its tissues, strong pressure quickly completes the process of formation of an intervertebral hernia. Therefore, this part of the spine and specifically the L4 L5 disc is the most vulnerable place for the formation of pathology.
Forms and symptoms of the disease
L4 L5 disc herniation has several forms of manifestation, and each has its own symptoms.
There are also symptoms characteristic of any type of this hernia:
- increased pain when moving, defecating, eating;
- pain subsides when standing;
- autonomic disorders (increased sweating, increased dry skin, swelling of the ankles);
- severe pain in the lower back when trying to lift a straight leg while lying on your back, and immediate subsidence of pain when bending the knee of the raised leg.
| Title and description | Symptoms |
|---|---|
|
Foraminal hernia - the rupture of the fibrous ring is directed to the anterior part of the spine.
|
|
|
Paramedian hernia - a hernial protrusion protrudes from the left or right side, compressing the roots of the spinal cord.
|
|
|
Dorsal hernia - rupture of the fibrous ring occurs on the back side. The hernial protrusion is directed back towards the spinal cord.
This is the most dangerous type of L4 L5 disc herniation due to its close proximity to the spinal cord. It not only compresses and injures the body of the spinal cord, but also causes many difficulties in treatment |
|
|
Medial hernia (Schmorl's hernia) - the development of a hernia occurs inside the vertebrae.
|
It is asymptomatic. |
Treatment methods for hernia L4 L5
The choice of the correct treatment method for a L4 L5 disc herniation depends not only on the direction of the protrusion, but also on its size. That's why it is important to accurately establish all the parameters of the disease, which can be done with CT or MRI(conventional radiography provides insufficient information).
- A hernia up to 5 mm in size does not require hospitalization. The main method of treatment is special gymnastics and spinal traction therapy.
- Hernial protrusion up to 8 mm can easily be treated with conservative treatment, including drug therapy, gymnastics, massage and physiotherapy.
- A hernia up to 12 mm requires hospitalization in the acute period and strict bed rest until the pain syndrome is completely relieved. Further treatment is carried out on an outpatient basis.
The operation is performed only if obvious symptoms of compression of the spinal cord or signs of a cauda equina appear (this is a complex of very severe symptoms in advanced pathology, including impaired urination, motor functions of the legs, etc.). - If the hernia is larger than 12 mm, urgent surgery is indicated.
Conservative therapy
Of primary importance in the treatment of L4 L5 disc herniation is reducing the load on this area. Therefore, in the first days of treatment, strict bed rest is required to ensure rest for the spine in a horizontal position.
The next stage of conservative treatment includes drug therapy:
- analgesics,
- non-steroidal anti-inflammatory drugs,
- muscle relaxants,
- chondroprotectors,
- vitamins,
- glucocorticoids.
After pain relief, the following treatment methods are added:
- physiotherapy (treatment with short and long electric waves, electrophoresis, ultraviolet irradiation);
- classes in the pool;
- massage;
- therapeutic exercises.
A mandatory component of therapy is wearing a rigid support corset. During the first months, the corset is worn constantly, and later it is worn while performing work related to lifting weights.
Features of therapeutic exercises
Gymnastics takes a leading place in the treatment of L4 L5 disc herniation. Special exercises relieve pathological tension in the back muscles, strengthen them, helping to support a weakened spine.
The insidiousness of a L4 L5 disc herniation is the imbalance it causes in different muscle groups: one of them is tight and tense, while the other is relaxed. Only a physical therapy doctor can take into account all the nuances and correctly prescribe the necessary exercises. All classes must be carried out under his direct supervision. Self-training without the supervision of a specialist can only aggravate the situation and lead to nerve pinching.
The main rule for performing exercises when treating a hernia of this department is to exclude axial load on the spine: these are all types of exercises in which the main pressure is placed directly on the spine, that is, on the axis of the body (squats, bends, swings and lunges). All classes are carried out in a lying position or on special inclined simulators.
(if the table is not completely visible, scroll to the right)

An approximate set of physical exercises for disc herniation L4 L5. Consult your doctor before doing this.
Click on photo to enlarge
Surgical intervention
The main goal of the operation is to release the nerve roots or part of the spinal cord from pressure. Today, four methods of surgical intervention are practiced:
Microdiscectomy is the removal of the disc herniation itself with minimal intervention in the human body. The most effective method.
Endoscopic hernia removal. The operation is performed without incisions through small punctures using special instruments. The surgeon monitors his actions using a monitor.
Implantation. During the operation, the surgeon completely removes the damaged disc tissue and installs an artificial implant in its place.
Nucleoplasty is a direct impact on the core of a damaged disc with cold plasma pulses. Through a small puncture, an image intensifier (electron-optical converter) electrode is inserted into the core of the L4-L5 disc, through which pulses are supplied. As a result, the nuclear tissue evaporates, the hernial protrusion decreases and the compressed nerve root is released.
Surgical treatment allows you to quickly relieve pain and restore the conduction of nerve impulses, but there is a high risk of relapse of the disease, since the very cause of the hernia remains unresolved.
Alternative Methods
Completely getting rid of the symptoms of the disease, as well as eliminating the main cause of disc herniation, is possible only with an integrated approach to treatment, which includes the following treatment methods:
- Hirudotherapy (treatment with leeches);
- Ozone therapy (injections of ozone preparations into the affected areas);
- Homeosiniatry (injections of homeopathic medicines into biologically active points responsible for the condition of the affected tissue).
Forget about the disease
The modern approach to the treatment of L4 L5 disc herniation is time-tested techniques combined with innovative methods of therapy. In 90% of cases, surgery can be avoided, damaged tissues are restored, and if simple preventive measures are followed, the disease never appears again.
Owner and responsible for the site and content: Afinogenov Alexey.
In more than half of the cases, intervertebral hernia affects the lumbar spine, especially its last segment, which is formed by the L4 and L5 vertebrae, as well as the intervertebral disc located between them. In 46% of cases, lumbar hernia is localized precisely in the L4 L5 segment.
A protrusion in this place can cause compression of the l5 spinal nerve. In this case, the innervation of the limbs is disrupted, sensitivity decreases, motor amplitude decreases, and muscles atrophy.
L4 L5 disc herniation is the most dangerous. It can disrupt the functioning of organs located in the pelvic area, limit motor activity, and cause partial or complete paralysis.
The disease manifests itself immediately after the formation of a protrusion: aching pain appears in the lumbar region and lower limb, lumbago, the leg goes numb, it is difficult to bend the knee, the foot partially loses its functions.
But don’t be upset: modern medicine can eliminate pathology without surgery and restore damaged areas of the disc by 80%.
Causes of pathology

The vertebrae located in the lumbar region differ from other vertebrae in their large size. In addition, their width is greater than their height. This feature is due to the fact that the heaviest loads fall on the lower back. In this case, the main burden falls on the last segment L4 L5. Therefore, even with the slightest disturbance in the nutrition of the intervertebral disc, the tissue structure changes and a hernia is formed.
Types of hernia
There are several types of hernia, differing in clinical manifestation.
Foraminal hernia
- The protrusion is directed to the front of the spinal column.
- Pain sensations develop only in the area of localization of the pathology.
- A mild tingling sensation is detected when laughing, sneezing, coughing.
Paramedian hernia
- The protrusion is noticeable on the right or left side.
- Pronounced pain in the affected area, radiating to the buttock.
- Rapid spread of pain to the leg.
- Numbness of the lower limb.
Dorsal hernia.
- It is especially dangerous because the hernia is very close to the spinal cord.
- The sensitivity of the lower extremities is impaired.
- Muscles become weak.
- There is uncontrolled excretion of urine and feces.
- Sexual function is impaired.
Medial hernia (also called Schmorl's hernia)
Shows no signs.
There are also symptoms common to all types:
- increased pain during physical activity, eating, defecation;
- relief of pain in a standing position;
- autonomic disorders (sweating increases, legs swell, skin becomes dry);
- unbearable pain if you try to lift your straight leg while lying on your back, and the disappearance of pain if you bend the raised leg at the knee.
Treatment methods

The choice of therapeutic methods depends on the type and size of the hernia. Therefore, the doctor refers the patient to a computer or magnetic resonance imaging scan.
Hernias with a diameter of less than 5 millimeters do not require hospitalization. They are treated with physical therapy and traction – spinal traction.
For a hernia whose diameter is within 5-8 millimeters, drug treatment, physiotherapeutic procedures, therapeutic exercises and massage are prescribed.
If the diameter of the hernia is in the range of 8-12 millimeters, then in case of exacerbation of the disease, hospital treatment and bed rest will be required. When the pain completely disappears, the patient is transferred to outpatient treatment. Surgery is prescribed only if there is severe compression of the spinal cord or signs of a “cauda equina” appear (this is the name given to the symptoms accompanying the advanced form of the disease: impaired motor function of the lower extremities, problems with urination).
If the diameter of the hernia exceeds 12 millimeters, then urgent surgical intervention is necessary.
Conservative treatment

First of all, you need to ease the load on the damaged area. For this purpose, the patient is prescribed bed rest and a corset is recommended. At first, the corset is worn constantly, and later - only when there is load on the lower back.
Then the doctor selects drug therapy, including:
- analgesics;
- non-steroidal anti-inflammatory drugs;
- glucocorticosteroids;
- muscle relaxants;
- chondroprotectors;
- vitamin complexes.
When the pain syndrome stops, drug treatment is supplemented with physiotherapy (UVR, electrophoresis, electrical stimulation), swimming, and therapeutic exercises.
Physiotherapy

In the treatment of L4 L5 disc herniation, physical therapy plays a leading role. It relieves muscle tension and strengthens the back muscles.
The peculiarity of the L4 L5 intervertebral disc herniation is that it causes muscle imbalance: some muscles relax, while others tense. Therefore, an experienced physiotherapist should select exercises and monitor their implementation. Self-study, instead of improving the condition, will lead to an exacerbation of the problem and pinched nerves.
Strengthen the back muscles and help return the intervertebral disc to its previous position.
Develops the muscles of the lower back, making them elastic. As a result, the flexibility of the spine increases and the general condition improves.
Surgical treatment
The main goal of surgery is to relieve nerve structures from pressure.
In modern medicine, 4 types of operations are used to treat hernia:
- microdiscectomy (the method is considered the most effective) – a hernia is cut out, minimally injuring the body;
- endoscopic treatment - the hernia is removed through small punctures (no incisions are made), all manipulations are controlled using a computer;
- implantation – the damaged disc is completely cut out and replaced with an artificial implant;
- nucleoplasty - a puncture is made in the skin, through which electrodes are inserted that deliver electrical impulses; under their action, the core of the disc is evaporated, freeing the nerve root.
Thanks to the operation, it is possible to quickly relieve pain and restore the conductive ability of the nerves. But it is unable to eliminate the cause of the pathology. Therefore, relapses are often observed after surgery.
Alternative techniques

Only comprehensive treatment can ensure complete recovery, which, in addition to traditional methods, also includes alternative ones:
- hirudotherapy – leeches are placed on the area where the hernia is located;
- ozone therapy – ozone preparations are injected into damaged areas using injections;
- homeosinia – homeopathic medicines are injected into reflex points.
The combination of innovative techniques with time-tested methods allows in 90% of cases to cure a herniated disc without surgery. And if you follow simple preventive measures, the disease will no longer remind you of itself.